Biomechanical & Physiological Underpinnings of Rehabilitation
Tissue healing biology
- Histology and biochemical characterization of Graft healing:
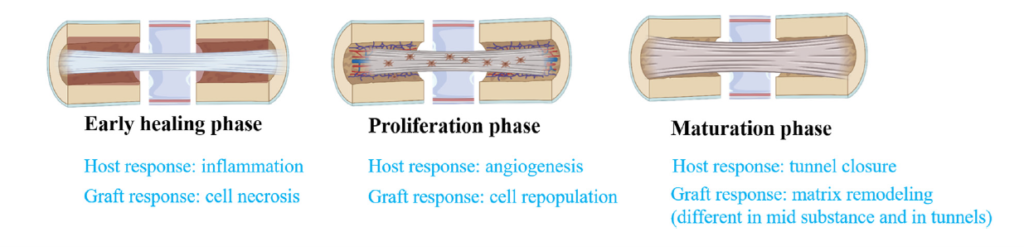
- Early healing phase saw the accumulation of neutrophils, TGFs, TNFs, macrophages, and IL-6 near the implanted graft. Many researchers believe that this graft underwent A-vascular necrosis, which started a cascade of growth factors due to cytokines released inside the tendon graft, while the outer side, exposed to synovial fluid with growth inhibiting factors, interferes with healing and causes massive collagen necrosis and disorganisation NSAIDs may impede ACL graft healing, according to recent research.
- Proliferation phase:
- Graft revascularisation is crucial for remodelling success. Oxygen deficiency from revascularisation failure necroses transplant tissue. Full revascularisation in 21 days to prevent cytokine-induced necrosis. Once the bone is drilled, numerous osteoblast cells on the joint’s periphery move towards the graft and create an interwoven network to shield it from synovial fluid, which is formed of B-type fibroblasts from the synovial membrane. The proliferation process included TGF, PDGF-AA, and PDGF-BB.
Maturation Phase:
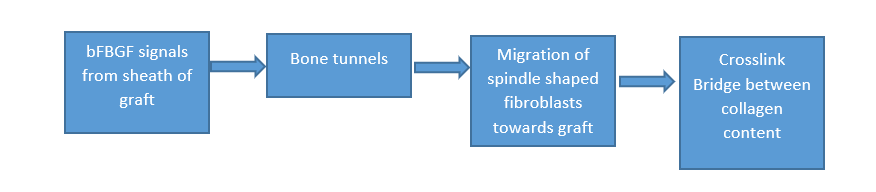
Due to BMP-2 and BMP-7, bone regrows like after fracture and helps repair graft to bone. Type 3 collagen is formed when basic fibroblast growth factors from the graft margin signal the bone tunnels to migrate spindle-shaped fibroblasts towards the graft to form a crosslink bridge and strengthen the graft and bone bond. These fibres are different in arrangement and diameter from pre-injury ACL fibres.
one of the researcher named Smith (Smith et al., 2011)conducted study in which he checked the laxity of the knee joint after ACL reconstruction from the day of surgery to 1 year. In this study, he found that the maximum laxity was found between the early healing and proliferation phase but there is no increase in anterior laxity was found between late proliferation phases.
Implication of loading after ACL reconstruction:
Asheesh Bedi examined whether early or delayed weight bearing after ACL reconstruction is beneficial. Unlike delayed weight bearing and mechanical axial stress, immediate weight bearing after ACL surgery may cause graft failure or delayed healing. Mechanical loading has been shown to help develop graft and bone after ACL replacement and joint homeostasis. Bedi et al. (2010). Thomoplous et al. found that mechanical loading helps bone tendon connection develop and succeed following flexor tendon surgery. (Thomopoulos et al., 2008)
Graft biology & graft choice relevance
Different approaches and multiple varieties of grafts are used for ACL reconstructions. It depends upon surgeons approach and preferences, gender, age, type of sports and athletic ability. Some surgeons prefer use of autograft in which tendon of patella or hamstring tendon are preferred and some prefer allografts of tibialis anterior tendon, patellar tendon and hamstring tendon.
• Autograft:
• Patellar tendon graft
• Hamstring tendon graft
• Allograft:
• Tibialis anterior tendon
• Patellar tendon
• Hamstring tendon
For the last decade, hamstring tendon and BTB autografts have been the most popular. Short- and long-term follow-up data demonstrates that allograft tendon has issues and even graft failure in certain patients, whereas autograft has donor-site morbidity, the main reason surgeons prefer autograft over allograft.(Foster et al., 2010)
Knee biomechanics after ACL injury/reconstruction:
In non-contact sports, excessive tibia anterior translation, valgus stress, knee internal rotation, low hip flexion angles, and high dorsiflexion angles damaged 50–80% of ACLs A partial ACL damage destroys some anteriomedial or posteriolateral fibres but leaves the rest to sustain the body. Spin (2010, Georgoulis et al.) observed bone bruising in roughly 80% of ACL injury patients’ medial femoral condyle 7%, medial tibial plateau 21%, and lateral 86% and 67%.
- ACL deficits cause initial swing phase internal tibial rotation but sufficient knee ROM. Tibia external rotation begins swings for people with intact or repaired ACLs.
In terminal stance, ACL damage patients had higher knee extension angles and less knee external flexion. - Damaged ACLs weaken quadriceps during mid-stance extension. ACL repair normalised all gait alterations.. (Georgoulis et al., 2003)
Quadriceps inhibition:
Weak quadriceps muscles after an ACL damage may cause dynamic instability, gait problems, knee extension issues, and muscular shortening, hindering post-operative rehabilitation. Many studies link quadriceps weakness to neural inhibition, arthrogenic inhibition, resting motor threshold changes, cortical inactivity, spinal reflexes, and joint proprioception. 2022 (Pietrosimone et al.)
- Recent research support therapeutic workouts that activate quadriceps muscles by mechanoreceptor stimulation, resulting in voluntary contraction and activation.
- OKC exercises with resistance training
- CKC strengthening exercises for hams and quads.(Sonnery-Cottet et al., 2019)
Neuromuscular deficits post-injury:
There are several knee proprioception ACL mechanoreceptors. ACL damage alters proprioception and somatosensory. Test this by passively moving the patient’s leg to a specific range and then asking them to actively return it. Unlike ACL-deficient legs, healthy legs can regain knee position. ACL surgery patients have trouble extending their knees from a flexed posture. Extension allows patients to bend knees easily. Proprioception was modified by muscle afferent nerve fibres when joint location changed. A bigger joint proprioception-repositioning mismatch reduces performance.(Ingersoll et al., 2008).
Load-tolerance & mechanotransduction: how progressive loading influences collagen alignment and graft remodeling — link to exercise prescription.
Inflammatory phase
Modulate Inflammation and Promote Vascularization:
ACL transplant recovery requires passive ROMs such partial weight bearing with axillary crutches and knee braces to maintain surgery site and passively move patella, retrograde massage, early vascularization, and inflammatory treatment. Biomechanical stimulation by mechanoreceptors causes intracellular reactions and cytoskeletal rearrangement. Extracellular signal-regulated kinase controls gene expressions and releases neutrophils, macrophages, and lymphocytes that infiltrate cytokines and VEGF to induce angiogenesis and maintain oxygen and nutrition supply to mend grafts.(Kacprzak, 2025).
Proliferative phase
Activates Growth factors:
Mechanical loading plays very important role in triggering the mechanical receptors which enhances the level of Insulin like growth factor and platelet derived growth factor which in turn enhancing the alignment of collagen fibers and promoting biomechanical properties.
Regulating Extracellular Matrix remodeling:
It changes the expression of matrix metalloproteinases (MMPs) and their tissue inhibitors in order to keep the extracellular matrix (ECM) in balance between synthesis and breakdown, which is important for proper tissue healing.
Activates growth factors
- Post-hamstring transplant patients should avoid high weights and prioritise partial weight bearing.
- Post-meniscus repair patients should avoid bending and Close Kinetic Chain activities.
- Always check the surgeon’s notes for patient recommendations and fixation strength.
.(Wang, 2013 #86).
Remodeling Phase (Several months to years)
Collagen alignment and maturation:
When a cell is mechanically stressed, its surface integrins link with ECM proteins and activate FAK, ERK, and RhoA/ROCK pathways (Humphries et al., 2006). These signalling cascades modify the cytoskeleton and produce genes that manufacture and arrange collagen, ensuring that collagen fibres can withstand knee stress..
Ligamentization:
Collagen fibres align with tensile stresses under mechanical loading, enhancing graft biomechanics. Mechanical stimuli activate integrin-mediated focal adhesion kinase (FAK). Mechanical stress activates FAK, ERK, and RhoA/ROCK via cell surface integrins and ECM proteins. These signalling cascades reorganise the cytoskeleton and express genes that make and align collagen to protect the knee from movement trauma.
1) Key Controversies in ACL Rehabilitation: A Concise Overview
1) Open-Chain vs Closed-Chain Exercises — Still No Clear Winner
The debate
Early open-chain knee extensions were formerly avoided due to graft stress. Closed-chain exercises like squats and leg presses look safer. Recent study suggests that well-controlled open-chain exercises may strengthen quadriceps without damaging the graft.
What the evidence shows
Findings are still unclear since the trials were planned differently, including when, how much, and what sort of workouts were done. Open-chain exercises with different loads have been done 2–12 weeks post-surgery, making standardisation difficult (Pamboris et al., 2024).
Implications for practice
- Do closed-chain exercises first.
- Add open-chain quadriceps exercise with light weights and limited ranges at weeks 4–6.
- If meniscus repaired, wait longer.
Key point: Open-chain exercise is not harmful by default — execution and timing matter more than the exercise itself.
2) Accelerated vs Conservative Progression — More Complex Than It Appears
The debate
Accelerated therapy accelerates weight-bearing, range-of-motion, and activity. Too much weight on the graft too rapidly might induce slippage and tunnel expansion.
What the evidence shows
Accelerated and cautious therapies usually provide similar long-term benefits. According to studies, early high loads and vigorous exercises may cause laxity. Comparisons are challenging due to different definitions of “accelerated” recovery. (Patra et al., 2022).
Implications for practice
Criteria, not time, should guide therapy when the
- Reduced swelling
- Complete knee extension
- Adequate leg control
- Quadriceps activation
Important: Proceed when the knee is ready, not planned. (Beynnon et al., 2011).
3) How Much Load Is “Right”? — The Largest Evidence Gap
The debate
Progressive loading helps tissue adapt, however the optimal load, repetitions, and joint angles post-ACL repair remain unknown.
What the evidence shows
Most of the information originates from animal studies, and few human studies directly examine tissue response. Clinicians use clinical symptoms and functional goals rather than biological prerequisites.(Gögele et al., 2025).
Implications for practice
- Start with small loads and controlled repetitions
- Move on to moderate endurance training
- Avoid twisting and rapid speeds
- Stop exercising if you notice pain, swelling, or redness.
Key point: Don’t assume your knee will react to load progression.
4) Graft Type and Surgical Factors — No One-Size-Fits-All Approach
The debate
Early loading may weaken hamstring grafts.
- Patellar tendon grafts may worsen front-knee pain.
- Meniscus or cartilage repair affects weight bearing.
What the evidence shows
Numerous studies focus on graft type while neglecting fixation and operation, hence limiting generalisation.(Banovetz et al., 2023).
Implications for practice
Load cautiously after hamstring grafts.
- Reduce knee flexion and CKC loading after meniscal repair.
- Always follow the surgeon’s full directions and correction detail.
Key point: Surgery establishes early limitations, and treatment must follow them.